A controversial new technique to improve the quality of eggs from older women undergoing IVF is being developed by Japanese scientists.
Because the procedure involves using eggs from two women to create a single viable egg for fertilisation, it has sparked a media furore over the potential creation of what have been inaccurately dubbed 'three-parent embryos'.
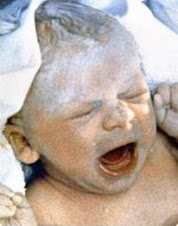
The success rate of IVF declines dramatically as the age of the woman undergoing the procedure increases. One of the reasons for this is thought to be the accumulation of abnormalities in the cytoplasm (the jelly-like substance that surrounds a cell's nucleus) of eggs from older women. Researchers at the St Mother Hospital in Kitakyushu, Japan, took the nucleus out of an egg cell from an older woman undergoing IVF and transplanted into an egg donated by a younger woman (under the age of 35) which had first had its nucleus removed. The resulting egg had the nucleus from the older woman but the cytoplasm from the younger woman.
The research team presented their results at the American Society for Reproductiove Medicine meeting in Atlanta, Georgia in October 2009. Out of 31 eggs on which the procedure was performed, 25 appeared to have transplanted successfully and looked healthy and so were used for fertilisation. Out of these 25 eggs, seven (28 per cent) formed early-stage embryos after being injected with sperm. This was a dramatic improvement on the usual three per cent success rate for the fertilisation of eggs from older women.
In this case, the embryos were not implanted back into women, but team leader Dr Atsushi Tanaka told New Scientist magazine: 'If we could transfer these constructed new embryos, I believe the success rate would be high'.
Although the vast majority of human DNA is contained inside the nuclei of cells, a handful of genes - just 37 genes out of around 25,000 genes in total - are found in the mitochondria, tiny structures that exist in the cytoplasm and provide power to cells. The embryos created by Dr Tanaka and his team would inherit only these 37 genes from the younger donor of the empty egg and cytoplasm, and their remaining 25,000 or so genes from the woman who donated the egg's nucleus and the man who donated the sperm. For this reason, a similar technique of nuclear transfer has been proposed in order to enable women who have severe genetic disorders associated with mitochondrial genes to have children of their own without passing on their condition.
The use of this technique on eggs intended for implantation is currently banned in the UK. However, the new Human Fertilisation and Embryology Act recognises what it calls the 'devastating effects' of mitochondrial diseases and will allow for secondary legislation to sanction treatment of mitochondrial diseases should therapies be developed.
SOURCE: BIONEWS.ORG.UK
Subscribe to:
Post Comments (Atom)
| Powered By widgetmate.com | Sponsored By Digital Camera |






No comments:
Post a Comment