Major advances utilizing embryo genetic testing with in vitro fertilization (IVF) technology have led to many new and expectant families, as reported by Reproductive Associates of Delaware (RAD) in their recent presentation at the October national meeting of the American Society for Reproductive Medicine in Denver, CO.
"This is a milestone of progress," noted Ronald F. Feinberg MD, PhD, the Center's IVF Medical Director. "We have merged our latest IVF techniques with successfully testing all 24 chromosomes within an embryo before it is placed back in the mother's uterus."
RAD's study demonstrated that almost 50% of 167 well developed and normal-appearing blastocyst embryos contained major chromosome defects, all of which were incompatible with normal pregnancy. The technology was applied to 26 patients who had previously suffered with miscarriage, unexplained infertility, and/or prior IVF failure. Preimplantation Genetic Screening (PGS) with blastocyst trophectoderm biopsy was the technique utilized.
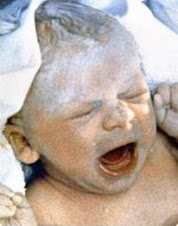
Following PGS, 71% of patients who were found to have at least one normal embryo achieved a successful pregnancy to date, despite previously negative outcomes and poor prognosis. One RAD patient that had never been pregnant had very few normal embryos via PGS. However, she successfully delivered healthy twins earlier this year after having two normal embryos biopsied via PGS and later placed in her uterus. All of the other PGS pregnancies at RAD have been singletons, following placement of just one normal embryo.
"We likely have a new and important reason for offering IVF and PGS to patients with infertility, prior IVF failure, and miscarriage", said Marc Portmann, Director of Lab Technology and Innovation at the RAD Center, who was also the lead author of the study. "This advance in IVF is of great significance because it will improve success rates, foster increased confidence in single embryo transfer, and will lower costs and risks of IVF." Many authorities within the field believe PGS could be applied to all patients undergoing IVF, but the larger benefits need to be fully evaluated.
Though many consider IVF and PGS to be expensive treatments, RAD's physicians believe this should be weighed against other factors, such as the health, emotional, and societal costs associated with infertility and miscarriage. High risks and costs of multiple gestations caused by other suboptimal treatments, including the transfer of multiple embryos during typical IVF procecures, must also be considered.
Approximately 15-20% of reproductive age women and men attempting pregnancy have infertility, a miscarriage history, or have experienced both.
source:sfgate.com