Broke, babyless and in need of help. John Naish examines the taboo question of how couples cope when it all goes wrong:
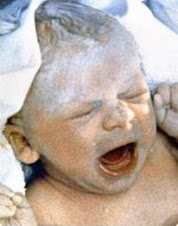
Across Britain next Friday, thousands of couples will brace themselves for a welter of “miracle-baby” stories as the world marks the 30th birthday of Louise Brown, the first test-tube child. In the shadow of assisted conception's many successes are the 75 per cent of women patients for whom the gruelling medical process never works. The vast majority are neither monitored nor offered counselling but, it seems, are expected to slink away, marked “failed.”
Caroline Gallup is among the 25,000 women each year whose fertility treatment proves fruitless, often after spending all their available funds and putting their relationships under perilous strain. Rather than quietly grieving, Gallup is campaigning for the NHS and high-earning private clinics to give support after assisted conception has failed and to fund studies into what happens to these people's lives.
Very little research has been done, but in 2000 a small study of 76 women by the Royal Maternity Hospital in Belfast found that five years after their unsuccessful treatment they suffered “significant psychological dysfunction”, particularly stress and depression. The research, published in the journal Human Fertility, concluded: “There is a strong need to prepare women better for treatment failure and to ensure that counselling is available when further treatment is no longer appropriate.” This echoes the findings of a Hull University study three years earlier. Both recommendations have fallen on deaf ears.
The government watchdog, the Human Fertilisation and Embryology Authority, says that it sees issues about follow-up monitoring and counselling as outside its remit, because it regulates only the process of infertility treatment itself.
Hence Gallup's campaigning. “I see the routine provision of post-treatment counselling as a moral duty,” says the 44-year-old Londoner. “When you are treated, you have to believe that a baby will grow. When it doesn't, the crash is awful, but you're buoyed as long as you can go through another cycle. I think it's only morally right for clinics to carry on with ‘after-sales service' when that hope has disappeared.”
COUPLES HAVE THE UTMOST OPTIMISM
“The clinics do tell you at their open days that there is a 76 per cent failure rate across the board, but couples aren't in a position to take that in,” says Gallup. “The only way you can enter into something so grim is with the utmost optimism.” Indeed, a study in The Obstetrician & Gynaecologist journal found that although clear information on success rates is given to couples, “the majority believe that they will be the minority who achieve pregnancy”.
Gallup and her husband decided to stop trying after they had paid £8,000 for private treatment. “It was partly down to money - we'd run out - and partly the fact that it was wrecking our relationship. My husband said he didn't want to go through it any more. It was turning me into a total obsessive,” she says, adding: “Blame can play a really big part in relationships after treatment failure. It's one of the big reasons why counselling is needed.”
Four years after the treatment ended, she says: “My husband and I are still dealing with it. I have had to reinvent myself. I didn't know what my identity was after we had finished. That's a huge psychological thing.” Now she has taken a less demanding job in her career in events management to spend time lobbying interest groups and politicians. She is also trying to develop a career as a writer, having published a book on her fertility treatment experiences, 'Making Babies the Hard Way.'
Emerging from fertility treatment babyless, broke and in need of professional support to get back on the rails is a common experience, according to the British Infertility Counselling Association. “A lot of people come out of the process highly stressed and they think they can go for free counselling, but there is no such thing,” says a spokeswoman. “Funding is a big problem for most people. They may well not be able to pay for private counselling because they have spent all their money on treatment.”
One of the few organisations to provide social support is More To Life, which helps involuntarily childless people to develop networks and swap advice. Membership costs £20 annually and has grown rapidly in the two years since it was established, says Susan Seenan, one of the organisers. “Social life can be difficult for infertile couples, especially women,” she says. “Wherever you go - barbecues, parties, christenings - everyone has children.
“It's difficult to talk about infertility and childlessness. It's seen as a stigma. But with more people leaving it until later in life to try for children, there is bound to be more infertility, more treatment, and more disappointed couples.”
It is not only infertile women who face bereavement and loss of purpose. David Downage regularly attends More To Life social events. He and his wife went through treatment in the NHS and privately, but ultimately decided that their hopes were beyond slim. “It was a traumatic decision, but the danger is that you go on trying too long and damage your relationship,” he says. “So we decided to move on.”
The Downages joined More To Life to extend their social network beyond old friends with their new families. “We had to find it by searching the web,” he says. “It's strange that clinics can't point you to organisations like this after the treatment has failed,” says David, 47, a property developer. “For a man, discovering that you're going to be childless raises questions about what you are doing with your life. Once you can pay the bills, what is there after that? My wife and I came to view it as an opportunity to do other things. She is keen to get involved in charity work with children. We plan to retire early and, hopefully, be able to put some of our money into building children's schools. Certainly we will be able to do that as a legacy.”
Finding renewed purpose is one of the best survival strategies, says Jacky Boivin, a researcher at Cardiff University's School of Psychology. She has followed more than 100 women undertaking IVF over seven years, and is running a five-year study of 818 couples in Denmark.
“There is not much research into what happens to people in the long term after unsuccessful treatment, but our data indicates that about 40 per cent of couples are highly distressed at having to stop. After they have made the decision, around 5 to 10 per cent remain stuck in that state. People who come to the end of the IVF treatment and feel they could have had more are often seized with resentment.
“You have to reinvent a life that is not about having a family,” she stresses. “You have to look for the positive while acknowledging the negative. People have to regain a sense of control over their lives, after having it taken over by regimens that tell them exactly when they should be having sex. And they need to look at the experience as an opportunity to renew life interests. Sadly, the lack of post-treatment counselling means people don't have support in this.”
AND NOW THE GOOD NEWS
There is one surprise. Boivin says: “Oddly, the divorce rate is much lower among couples whose fertility treatment failed than for the general population: 10 per cent versus 50 per cent. We don't know why. There is life after infertility treatment. Not always an easy one, but most people will go on to find contentment, though the experience will always carry a sting.”
SOURCE: THE TIMES ONLINE
Subscribe to:
Post Comments (Atom)
| Powered By widgetmate.com | Sponsored By Digital Camera |






1 comment:
Post a Comment