Sunday, July 27, 2008
The birth that started a revolution
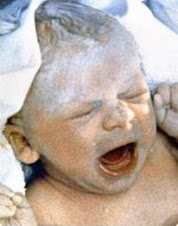
Thirty years ago Louise Brown, the first test tube baby, was born, and the world of fertility changed forever.
Her mother, Lesley, 33, had blocked fallopian tubes, so Dr Patrick Steptoe and Bob Webster took an egg from one of her ovaries, under anaesthetic, and fertilised it with sperm from her husband, John, in a laboratory, before placing it in her uterus. Nine months later, on July 25, 1978, Louise was delivered by Caesarean section at Oldham and District General Hospital.
Since that day, a series of in-vitro fertilisation (IVF) breakthroughs has enabled tens of thousands of couples to have the children they longed for. Other leaps have included treatments for male infertility, the use of donor eggs, surrogates and the genetic screening of embryos.
In Britain alone, 111,633 children have been born through fertility treatment; worldwide, the figure is estimated to be 3.5 million. The latest figures from the Human Fertilisation and Embryology Authority (HFEA), the regulatory body set up in 1991, show that 32,626 couples in Britain had IVF in 2005, leading to a total — including twins and triplets — of 11,262 children. About 25 per cent of IVF treatments are funded by the NHS; the rest are paid for privately, costing up to £8,000 (Dh58,525) a cycle.
Exceptions: But while IVF has answered the prayers of many couples, it is not a cure-all. The average success rate nationally for women under 35 is 29.6 per cent, while those aged between 40-42 have just a 10 per cent chance of conceiving using their own eggs. (There are exceptions: at the Assisted Reproduction and Gynaecology Centre in London, for example, the take-home baby rate is 59.9 per cent for women under 35). And fertility treatments are also transforming the family, raising ethical questions about concepts such as “saviour siblings”, babies genetically matched and created to provide tissue — often umbilical cord stem cells — to treat disease in an older child.
Similarly, treatment for post-menopausal women, same-sex couples and the spectres of sex selection for social reasons (illegal in the UK) and “designer babies”, where embryos are chosen or discarded for reasons other than health and viability, have also led to disquiet. Meanwhile, Louise, has a child of her own. Cameron, aged 18 months, was conceived naturally — an everyday miracle perhaps, but no less a miracle for that.
The first IVF triplets were born in 1984. In recent years, the HFEA has raised concern over the relatively high incidence of multiple births conceived through IVF; the risk of death before birth or within the first week after birth is more than four times greater for twins, and almost seven times greater for triplets, than for single births. Currently, around one in four IVF pregnancies results in twins or triplets, and the HFEA is now calling for more single embryo transfers to reduce this figure to 10 per cent —although clinicians are reluctant to do so, as replacing just one embryo reduces the chance of pregnancy. Mindy Vernon, 44, and her banker husband James, 43, live in Sevenoaks, Kent. They have triplets William, Thomas and Katherine, aged seven. “James and I got married when I was 32 and we tried for a year and a half to have a baby, without any success. Medical tests revealed no major issues and when the doctors diagnosed unexplained infertility, we decided to go for IVF. We had three rounds of treatment at Shirley Oaks hospital, at a cost of £2,000 a cycle, which failed. By the fourth cycle we were really losing heart, so we had three embryos replaced instead of the two we'd done previously. “Around the time of the IVF transfer I had terrible backache, so I had acupuncture treatments for the pain. When I mentioned that I was having fertility treatment, the practitioner said she could treat that, too, by inserting the needles at other sites on my body. Multiple pregnancy risk “I know there's conflicting opinion about whether acupuncture increases the success of IVF.
It may just have been coincidence, of course, but in my case it really did seem to work. “When we were told we were expecting triplets, we were overjoyed that I was pregnant at all and we didn't immediately take in the significance of what it meant to be carrying three babies at once.
Only later did we learn how much riskier it was for both me and the babies; we were informed that they might not all survive and were given a choice of terminating one of them. But after talking through the pros and cons, we knew we wanted to keep all three. “I have always felt it is important to keep fit, but I was told not to exercise and to eat as much as I could, so I stuffed myself and put on five stone.
I wasn't anxious during the pregnancy, because I had faith in my body and faith in the medical staff who were looking after me. I had a really easy pregnancy, too; I wasn't badly affected by morning sickness. “I gave up work at 22 weeks, and at 26 weeks my consultant advised me to go to hospital and stay there, so I could have complete rest and be monitored twice daily in case any problems arose. I knew I was having two boys and a girl, which the hospital had named A, B and C, and I spent my time listening to classical music and visualising them as individual little people.
“My mother was cooking for me at home every day and bringing food into the hospital, so I sat around getting fatter and feeling very special and quite serene. The babies were finally born by C-section at 34 weeks — a team of 21 doctors and nurses was involved in the delivery.
None of them had any medical problems at birth, or subsequently. “They were allowed home after three weeks, by which time they had put on weight — and then the work really started: I breast-fed them as best I could for two months, but I didn't have much milk so they also got through 24 bottles a day. “James and I were lucky to have lots of support from my mother, in particular, who stayed with us for a whole year, and in the first few months James's mum crossed half the country every weekend to help out. “My mother and I did the weekday shifts and James and his mother took over at weekends so we could rest. Those early days, months and years were utterly exhausting and looking back, I can't believe we managed, but somehow we did. Having triplets is a joy, but it's also emotionally and financially draining.
Not convinced “I feel ambivalent about the guidelines that only two or even just one embryo should be replaced. There's no doubt that replacing three embryos maximises a woman's chances of getting pregnant, but it's not without its medical risks and bringing up three babies is not for the fainthearted. Still, we were fantastically lucky with our three; we love them dearly and wouldn't swap them for the world.”
The first commercial surrogacy took place in Britain in 1985 when Kim Cotton, a mother of two, was paid £6,500 to carry a child conceived using her egg and the infertile woman's husband's sperm. It is now illegal for a surrogate to charge fees, but reasonable expenses may be paid to cover clothing, travel, food, time off work, etc, amounting to anything from £7,000 to £15,000.
Two types of surrogacy: There are two types of surrogacy. Straight surrogacy uses the egg of the surrogate and the sperm of the intended father and is usually carried out via artificial insemination at home. Host (or gestational) surrogacy requires IVF, as embryos are created using eggs and sperm from the intended mother and father and transferred into the surrogate mother. Fiona O'Driscoll, 38, who works for the charity Save the Children, is married to Andrew, 39, a business consultant. A surrogate mother is carrying their baby, due in October. “I have a condition called Mayer Rokitansky Kuster Hauser Syndrome (MRKH), which means I was born without a womb — although I do have ovaries — so I knew that if I wanted a family I would need to use a surrogate mother or adopt. We looked at adoption, but it's almost impossible to get a baby, and we really wanted to create one that is genetically ours. “We got in touch with the non-profit organisation Surrogacy UK in order to make contact with a surrogate and find out more about the process. The ethos is one of friendship before surrogacy and, at the social events, we got to know another couple, Kate and Dennis, really well over a period of months. They already have two children and offered to help us. “To be honest, my first instinct was: ‘Why on earth would someone offer to carry another woman's baby?' It was hard to believe anyone would do something so momentous purely out of the goodness of their own heart. But Kate is such a selfless person and she's certainly not in it for the money; all we do is make sure she's not out of pocket by covering expenses like multivitamins and maternity wear, taxis and childcare. “We were treated at the London Fertility Clinic in Harley Street; I took drugs to stimulate my egg production. These were fertilised by Andrew's sperm, and the resulting seven embryos were frozen. Two survived the thawing process and were transferred into Kate, who had taken drugs to prepare her body. Two nail-biting weeks later, Kate, Andrew and I were all together in a coffee shop in central London when the call came through that she was pregnant and we all burst into tears. “Kate is now 28 weeks pregnant. Andrew and I — and Dennis — will all be at the birth; it's very exciting. We're so proud of what they are doing. You read horror stories about surrogacy costing a fortune or the surrogate trying to keep the baby, but the truth is, it's about a good friend giving you the most extraordinary gift imaginable.”
Names have been changed
SOURCE: Daily Telegraph
Subscribe to:
Post Comments (Atom)
| Powered By widgetmate.com | Sponsored By Digital Camera |






1 comment:
I'm an acupuncturist and find that the key to combining acupuncture and IVF successfully preparation. I recommend taking 3-6 months and working with an experienced acupuncturist that utilized personalized herbal formulas, regular acupuncture treatments, charting, dietary therapy and lifestyle counseling.
Doing a few acupuncture treatments during an IVF cycle may increase the success rate 20-25%, but properly preparing for an IVF cycle may increase the success rate 100-200%. These are stats from my experience in the clinic.
Post a Comment